Considering Enteral Feeding Route
The following need to be considered by the interdisciplinary team (Corkins, Balint, Bobo, Yaworski, & Kuhn, 2015) when choosing the most appropriate enteral feeding route:
- risk of aspiration (see Table 1 )
- considerations specific to the child’s medical condition, gastric function or previous surgeries
- expected duration of enteral feeding
- needs and desires of the child and family
The decision regarding the most suitable enteral feeding route is generally made by the physician and interdisciplinary team in collaboration with the child and family. The dietitian should be involved with the decision-making process based on knowledge of current intake from oral and/or enteral nutrition sources, tolerance, and nutrition requirements.
Enteral feeding tubes are described by where they enter the body and where they deliver the enteral feed. When safe to do so, gastric feeding is preferred over jejunal, as gastric feeding tubes are easier to place and offer more physiologic feeding compared to transpyloric (i.e. jejunal) feeding (Corkins, Balint, Bobo, Yaworski, & Kuhn, 2015); (Braegger, Decsi, Dias, Hartmann, & Kolacek, 2010).
- nasoenteric tubes (or simply called nasal tubes) are inserted through the nose; nasogastric tubes are nasal tubes that deliver feed into the stomach, while nasojejunal tubes are nasal tubes that deliver enteral nutrition to the jejunum (small intestine)
- gastroenteric tubes are feeding tubes that are surgically inserted through a stoma (gastrostomy) into the stomach. A gastrostomy tube typically provides enteral nutrition into the stomach, whereas a gastrojejunal tube delivers the enteral nutrition into the jejunum
- A jejunal tube may be surgically placed through a stoma called a jejunostomy to enter and deliver enteral nutrition directly into the jejunum. Jejunal feeding is indicated when gastric feeding is not possible or tolerated, such as with aspiration, gastroparesis, gastric outlet obstruction, or abdominal surgery
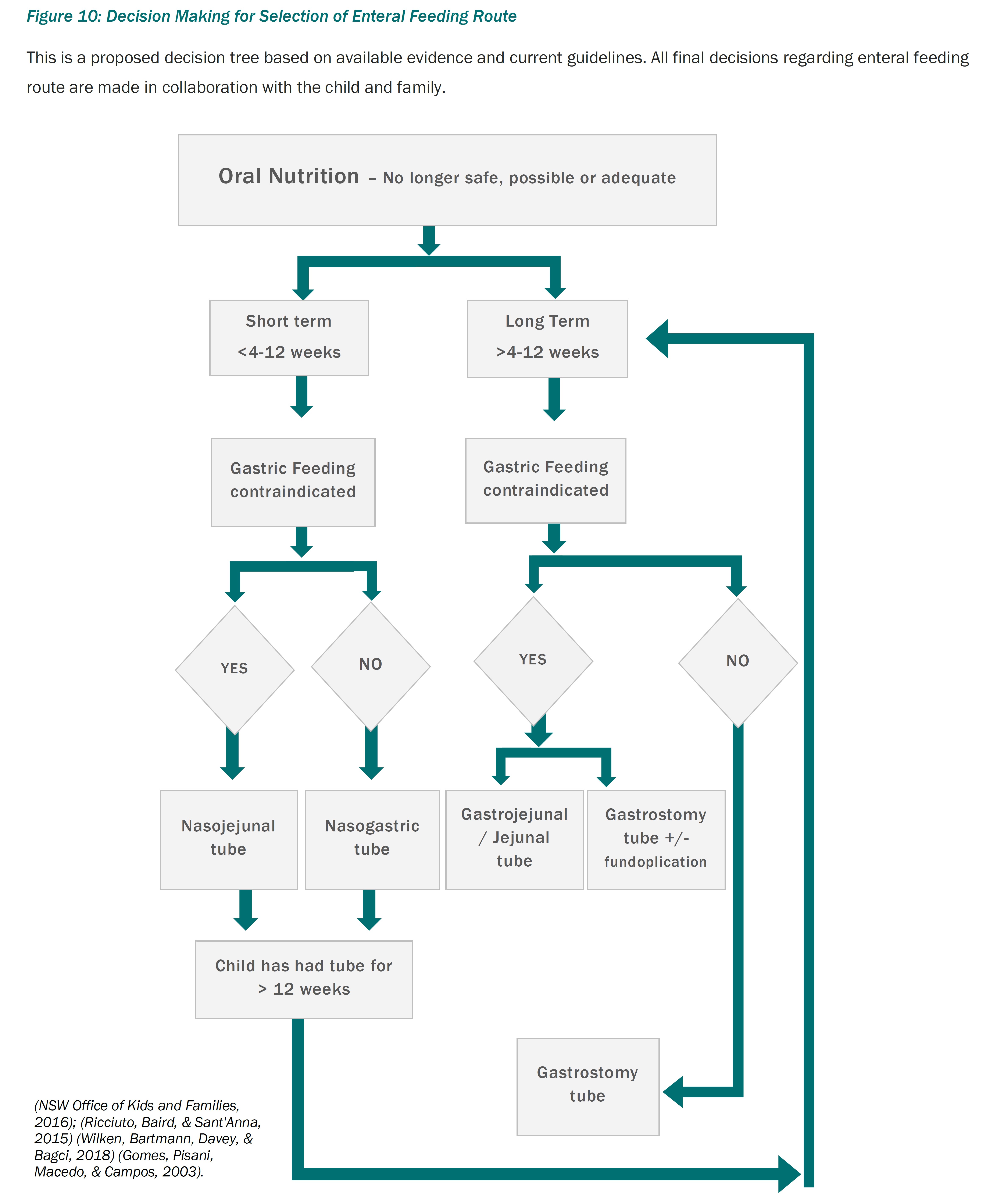
The use of nasal tubes is considered primarily for temporary or short-term enteral nutrition support. Consideration of gastrostomy insertion for longer duration of enteral support is highly recommended when enteral feeding is expected to extend beyond four to 12 weeks. Selection of the most appropriate enteral feeding route can be guided by the decision tree in Figure 10. Tube specific care recommendations regarding nasoenteric tube size, measuring, taping, and placement checks are provided by the home enteral nutrition support programs.
Although inconclusive, increased food aversion has been noted in children using a nasogastric tube for greater than three months, compared to those who used it less than three months or those with a gastrostomy tube (Ricciuto, Baird, & Sant'Anna, 2015).
- late preterm infants are more likely to exhibit oral sensorimotor sensitivity and facial defensiveness in later infancy if they received more than three weeks of enteral nutrition using a nasogastric tube (Dodrill, et al., 2004)
- in contrast, a recent study found no difference in food aversion behaviours in children with established tube dependency regardless of the use of a nasal or gastrostomy type tube (Wilken, Bartmann, Davey, & Bagci, 2018). However, it should be noted that many of the children in both groups had experienced nasogastric tube feeding for longer than three months
- in the absence of a randomized controlled trial, which is not feasible, the role of nasal tubes in the development of food aversion and tube dependency cannot be known, but factors such as painful reinsertions and quality of life, are highly relevant
- furthermore, in adult patients, the use of nasogastric tubes, as opposed to gastrostomy tubes, has been associated with increased risk of gastroesophageal reflux and aspiration pneumonia, likely also relevant for children with dysphagia who require more than short-term enteral support (Gomes, Pisani, Macedo, & Campos, 2003), (Alnassar, Oudjhane, & Davila, 2011).
Physicians and the interdisciplinary team should provide information and guidance to parents and children (as appropriate) early in the treatment process. This communication will assist and support decision-making which is based upon current practice recommendations, family preference, and the anticipated duration of enteral feeding (ESPGHAN Committee, 2010); (National Institute for Health and Care Excellence, 2006); (European Society of Parenteral and Enteral Nutrition (ESPEN), 2005); (Canadian Paediatric Society, 2009), (Spanish Society of Parenteral and Enteral Nutrition (SSPNE), 2011).
Children who are fed by a nasoenteric tube should be reviewed by the interdisciplinary team, with the child and family, within 4 to 12 weeks to discuss the ongoing management and consideration of transition to an alternate feeding tube, e.g. gastrostomy, jejunostomy, (Boullata, et al., 2017); (Dunitz-Scheer, et al., 2009); (Corkins, Balint, Bobo, Yaworski, & Kuhn, 2015); (Braegger, Decsi, Dias, Hartmann, & Kolacek, 2010). As there are risks to both long-term nasoenteric tube use and gastrostomy tube insertion, it is essential to consider the child’s medical needs, overall health, ability to safely consume oral intake, and recent progress with feeding skills and oral intake (ESPGHAN Committee, 2010), and together determine the best option for the child in the short term, and the long term (as applicable).