Introduction
Background
Pediatric eating, feeding and swallowing difficulties are increasingly prevalent and often co-morbid with other conditions. For children with pediatric feeding disorder (PFD) and their families, it results in a significant impairment to family life including: time commitment, financial expense, psychological distress, morbidity and risk of mortality. There is a strong desire among families, healthcare, social services, and the education sectors to improve outcomes for this vulnerable population. It is widely acknowledged that systemic change and collaborative practice are needed in order to achieve these outcomes in this highly complex area of practice.
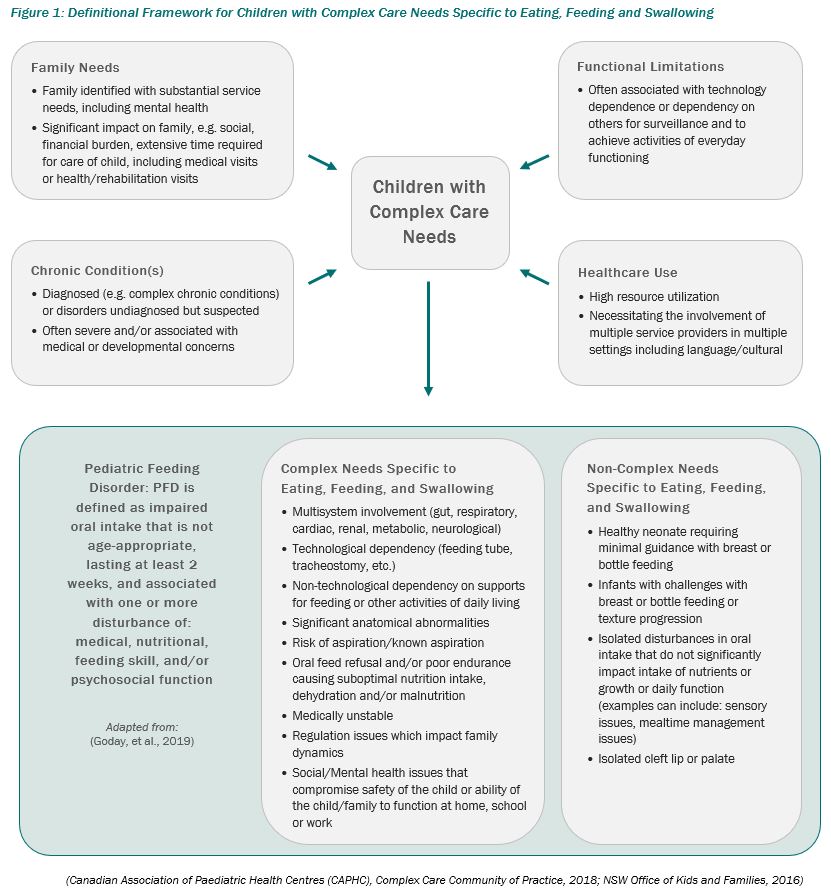
PFD may present in infants and children at any age. PFD can encompass all aspects of the child’s development including feeding and swallowing, oral motor skills, and sensory processing, as well as nutritional requirements, and feeding relationships. PFD commonly develops as a result of a variety of circumstances, often complex, that may occur early in a child’s life. Examples of complex and non-complex pediatric cases are listed in Figure 1.
In addition to its primary role of providing nutrition to support growth and development, a positive eating, feeding and swallowing experience takes place in an environment of parent or caregiver responsiveness, socialization, communication, sharing and nurturing. Likewise, the mealtime environment and practices may be influenced by the community and culture of the family and child (Evans Morris & Dunn Klein, 2000).
Aim
The Pediatric Feeding Disorder Clinical Practice Guide (CPG) is part of a quality improvement initiative with the purpose of standardizing and improving care for children with PFD in Alberta. The CPG aims to provide evidence-based clinical guidance to enhance quality of life and improve patient safety; these are pivotal to quality improvement in a field that has clinical and ethical complexity, and where very few guides and standards exist nationally and internationally.
Key Objectives
This guide provides information, guidance and recommendations, to support AHS healthcare professionals in making clinical decisions regarding the screening, assessment and management of children with PFD. The guide aims to:
- Facilitate processes for quality improvement to optimize quality of care and health outcomes
- Optimize psychosocial outcomes in families
- Facilitate a consistent approach as close to home as possible
- Facilitate communication and collaboration among healthcare professionals and with families by using consistent language, definitions and strategies
- Assist practitioner decision-making for a variety of populations
- Offer clinician tips, tools and training resources to support lifelong learning and education
Scope
This guide applies to infants, children and youth with PFD from birth to 18 years of age.
It offers a framework for screening, assessment and management strategies across the four health domains of medical, nutrition & hydration, feeding skill and psychosocial dysfunctions. Clinicians working with particular diagnostic groups should refer to other more specifically related documents together with specialists in these areas. This guide excludes traditional psychiatric eating disorders as defined by DSM5, e.g. bulimia, anorexia nervosa (DC:0-5 Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood, 2016), and picky eating.
Audience
This guide can be used by healthcare professionals working individually, or as part of a formal or informal PFD team. Healthcare professionals who may utilize this guide include (but are not limited to):
- community physicians
- dietitians
- gastroenterologists
- lactation consultants
- nurse practitioners
- nurses
- occupational therapists
- otolaryngologists
- pediatricians
- pharmacists
- physiotherapists
- psychologists
- psychiatrists
- respiratory therapists
- social workers
- speech-language pathologists
- surgeons
The topics and content of the guide are relevant for healthcare professionals across a variety of settings including: outpatient clinics, rehabilitation hospitals, community (including schools), home care environments, and urban and rural locations.
The area of PFD is a complex field requiring significant knowledge, practice, and experience. Clinicians should recognize and acknowledge their limitations in this area, and not work beyond the scope and competency of their practice. Where the need for skill development is identified, appropriate training, supervision and mentoring should be sought from an experienced healthcare professional in their field, or from an established pediatric feeding team.
Healthcare professionals should be aware of recent literature in their field, current best practices, relevant clinical competencies and their professional Code of Ethics. This guide provides a sufficient level of detail as to the considerations required for effective clinical reasoning, decision making and provision of service in the area of PFD inclusive of enteral feeding. It is intended that where adequate resources are not available in the local setting, the guide may be used to identify the need for onward referral or collaboration with more specialized services.
Methodological Quality of Clinical Practice Guide
This Clinical Practice Guide, as part of the Alberta Health Services (AHS) Pediatric Eating and Swallowing (PEAS) Project, was initiated in response to feedback from families and AHS healthcare professionals practicing in the area of PFD across Alberta. These stakeholders identified gaps in clinical knowledge and safety, and requested further education, guidance and standardization of screening, assessment and management of children with PFD.
The Standardized Practice and Education Working Group was established within the PEAS Project to facilitate the development of an evidence-based PFD clinical practice guide. Members of the working group were initially identified through an expression of interest process, with additional members invited to join the group as required. Group membership included speech-language pathologists, dietitians, occupational therapists, a psychologist, a psychiatrist, physicians, and nurses from the Alberta Children’s Hospital (ACH), Stollery Children’s Hospital (SCH), and Glenrose Rehabilitation Hospital (GRH), Community Rehabilitation, Home Care, and Community Care; with endorsement from the Maternal, Newborn, Child & Youth Strategic Clinical NetworkTM (MNCY SCN) Child & Youth Standing Committee, and in collaboration with Nutrition & Food Services, Health Professions Strategy & Practice, branches within the Government of Alberta, and families. The working group was chaired and provided project management support by AHS.
The scope of the guide was determined by the working group. Initially, a search was undertaken to identify any existing evidence-based guides which could be adapted for local use. The guide, Feeding Difficulties in Children – A Guide for Allied Health Professionals from the New South Wales of Kids and Families (NSW Office of Kids and Families, 2016) was identified as a very thorough document that could be adapted to include the Pediatric Feeding Disorder – Consensus Definition and Conceptual Framework (Goday, et al., 2019), and A Practical Approach to Classifying and Managing Feeding Difficulties article (Kerzner, et al., 2015). From there, an outline was created to reflect the Goday, et al. and Kerzner, et al. articles for screening, assessment and management of PFD, and was amalgamated with the NSW guide and adapted based on cultural and linguistic relevance, local information and resources. A broad review of both published and unpublished literature was completed from national and international sources. Data extracted evidence tables were created and where supporting literature was identified, the working group made recommendations based on the evidence, integrated with clinical expertise. Reference to supporting evidence is incorporated throughout the guide. Where evidence was not found, the working group made a consensus recommendation based on clinical expertise. An evidence classification scale was applied to the identified literature. The working group decided that the classification scale added no additional value to the guide and was therefore not included.
Rapid literature reviews were also conducted by an analyst on the AHS Innovation, Evidence and Impact (IEI) team. Research questions were designed based on consultation with members of the Standardized Practice and Education Working Group. The literature search strategy was developed in consultation with librarians within the AHS Knowledge Resource Services department, who then conducted the searches on behalf of the IEI analyst. Searches were limited to literature published in English between 2009 and 2019. Evidence was summarized in narrative format and then sent to the working group for inclusion during the guide development process. These reviews were not intended to be comprehensive systematic reviews; rather, they provided a snapshot of the existing evidence related to the topic at hand.
Additions or changes made to the NSW guide by the working group were qualified by using the Appraisal of Guidelines for Research & Evaluation II (AGREE II). The guide proceeded through the PEAS Working Groups, PEAS Leadership, and Steering Committee (internal and external stakeholders) for review and approval.
