Choosing an Appropriate Enteral Feeding Regimen
In order to enhance motility and nutrient metabolism in the child with an enteral feed, the preferred method of enteral feeding is by bolus feeding (Schanler, Shulam, Lau, Smith, & Heitkemper, 1999) (Patel, Piazza, Layer, Coleman, & Swartzwelder, 2005) (Rovekamp-Abels, et al., 2015). Enteral feeds can also be administered by continuous, intermittent/bolus, cycled or a combination of these, each method with its own advantages and disadvantages.
Refer to:
- Appendix 10 - Tube Feeding Schedules/Regimens for Enteral Feeding
- Figure 7 - Nutrition Support Decision Making Tree
- Provincial Enteral Nutrition Insite Page (AHS Staff Login required)
Table 11: General Formula Selection for Enteral Feeding
|
Feed Type |
Composition |
Indications |
Considerations |
|
INFANT FEEDING |
|
|
|
|
Expressed Breastmilk (EBM) |
|
|
|
|
Infant formula |
|
|
|
|
Pasteurized donor human milk (DHM) |
|
|
|
|
Extensively hydrolyzed |
|
|
|
|
Amino acid-based |
|
|
|
|
Specialty formula |
|
|
|
|
PEDIATRIC |
|
|
|
|
Polymeric – includes |
|
|
|
|
Semi-elemental |
|
|
|
|
Elemental |
|
|
|
| Blenderized or home blended food |
|
|
|
|
Modulars/Additives |
|
|
|
When choosing an enteral feeding regimen, consider the following (Bauer, 2002) (American Society for Parenteral and Enteral Nutrition Board of Directors, 2009):
- current medical condition, nutrition and biochemical status
- tolerance to any previous enteral nutrition regimens
- safety of ongoing oral intake to complement enteral feeding, general consumption
- child’s age, activity level, preferences, lifestyle, development, and family routine
- nutrition needs, and specific nutrient requirements for optimal growth and development, volume required to optimize tolerance, and water flushes to support hydration needs
- route of delivery and formula type
- refeeding risk
- expected duration of nutrition support
- cost effectiveness and/or implications
- parent ability to safely administer the regimen
- sustainability of the proposed regimen, e.g. complex routines may be ok for short-term success, but may not be sustainable for longer term intervention, requires reassessment
Enteral feeding should only be started following medical confirmation of tube placement. In most cases, enteral feeds can be started at full strength with the volumes being gradually increased in stages either as an increased infusion rate or as a larger bolus (Shaw & Lawson, 2007).
Consideration of advancing feeding regimens should be undertaken upon review of the above-mentioned factors. As feeds progress towards goal rate or schedule, the child’s tolerance and medical stability should be monitored.
Clinical condition, tube type, tolerance and family needs may influence administration of enteral feeds requiring an enteral pump (See Table 12). Continuous pump feeding is required for jejunal feeding due to the lack of reservoir capacity in the small bowel. Bolus feeds are contraindicated for jejunal feeding (Boullata, et al., 2017) (Braegger, Decsi, Dias, Hartmann, & Kolacek, 2010) (NSW Office of Kids and Families, 2016). Intermittent pump feeding may be possible and should be determined based on individual needs and tolerance. However, particularly for infants, consultation with the medical team is recommended due to potential risk of hypoglycemia when ceasing jejunal feeds (NSW Office of Kids and Families, 2016).
Table 12: Feeding Pump Criteria
| Medical indications requiring a feeding pump |
|
Required for management of:
|
| Indications for feeding pump discontinuation |
|
Examples:
|
| Non medically supported requests for feeding pump (and suggested responses) |
|
Education provided:
|
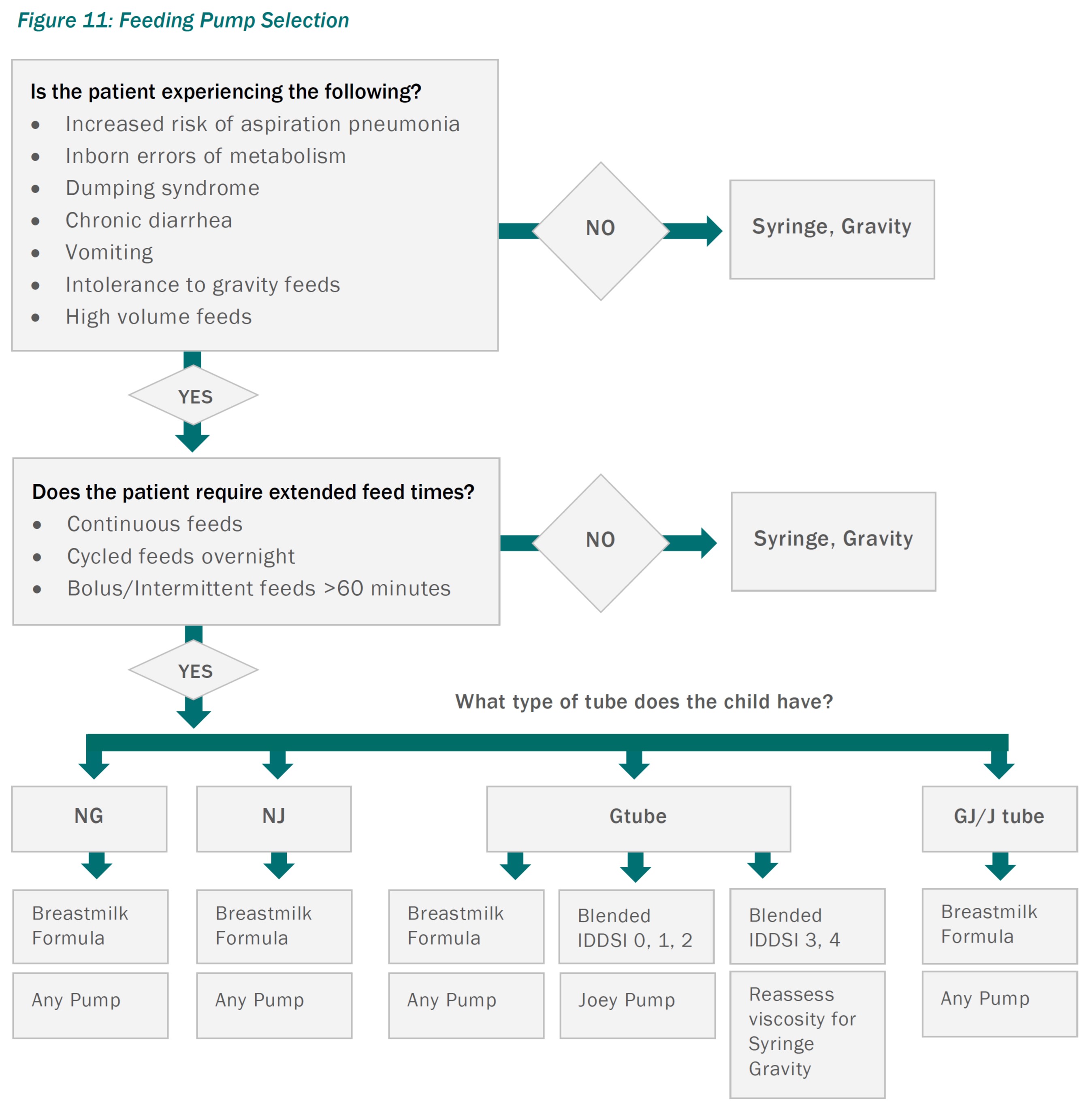
The indications for feeding pump use may change with time. A child should be reassessed and transitioned from a pump to gravity or syringe feed administration when the original indication for the pump has resolved.
